A Dietitian's Nutrition and Lifestyle Tips for Reducing Inflammation
Mar 02, 2022
Inflammation is the immune system's defence mechanism designed to protect us against disease, infection, injury, and even stress. In the short term, inflammation can help our bodies heal, however, long-term (ie. chronic) inflammation can lead to pain, illness, and poor health. In this article, the Registered Dietitians at Vitality Nutrition explore evidence-based strategies for reducing or entirely avoiding chronic inflammation using the power of diet and lifestyle!
If you are interested in listening to this discussion, we recorded a podcast that discusses these principles and lifestyle considerations in depth. You can find the episode here!
UNDERSTANDING INFLAMMATION
Before beginning a conversation on inflammation, it's important to distinguish between an inflammatory response that is 'acute' vs 'chronic'. Let’s explore the definition of each:
- Acute inflammation occurs when our body senses harm – such as an infection or immanent threat – and works to fight it off or protect our bodies in a short period of time. This is a normal response that promotes healing. Some symptoms of acute inflammation include pain, redness, swelling, and heat. For example, you experience acute inflammation when your muscles are sore from a workout, when you have redness and swelling around a cut, or if you have a sore throat from a cold or flu.
- Chronic inflammation is a lower-grade response that occurs over longer periods of time. Unlike an acute inflammatory response to a cut or injury, chronic inflammation can be connected to our environment, dietary choices, stress levels, and overall health. This form of inflammation can be harmful and may increase the risk of several diseases such as diabetes, cancer, arthritis, Alzheimer's disease, kidney disease and heart disease.
Adopting nutrition and lifestyle habits that achieve an anti-inflammatory effect is an important consideration in reducing chronic low-grade inflammation and in promoting your long-term health and vitality.
SIX NUTRITION PRINCIPLES TO COMBAT INFLAMMATION
You may have been directed by a healthcare provider to reduce chronic inflammation triggers in your life. Or perhaps you've read about the importance of these lifestyle decisions online. But have you ever considered consulting a Registered Dietitian to help guide this decision-making and planning process? Dietary patterns are a fundamental aspect to reducing chronic inflammation, and a Registered Dietitian will bring an evidence-based and individualized approach. While we strongly recommend working one-on-one with a nutritionist to determine the anti-inflammatory nutrition and lifestyle considerations that are right for you, we can start by reviewing six key nutrition principles that help fight inflammation:
1. SUPPORT YOUR GUT
Our gut is an ecosystem that trillions of microorganisms call home. Some of these microorganisms promote inflammation, whereas others are thought to reduce it.
Increasing one's fibre intake is a strategy that can encourage a more health-promoting profile of these gut microorganisms. Some sources of fibre include fruits, vegetables, beans, nuts, seeds, starches, and whole grains. Fibre comes in a variety of plant-based foods, with some examples of very high fibre sources shown in the infographic below:

In addition to fibre, fermented foods have also been shown by research to support the gut by improving the gut microbial balance. Examples of foods with live microorganisms (ie. fermented foods or foods or probiotic foods) that our Registered Dietitians love are pictured below:

What about dairy? Many clients ask our Dietitians whether dairy is an inflammatory food they should consider avoiding. While it is commonly proposed that dairy is a food that causes inflammation in the body, current research has not found a link between dairy consumption and increased inflammation, and has even found that dairy is associated with weak anti-inflammatory properties. Furthermore, fermented dairy, like Greek yogurt and kefir, may even be associated with decreasing inflammation by contributing favourably to the gut microbiome. However, if you have a lactose allergy or intolerance, consuming dairy will increase markers of inflammation. As Registered Dietitians, we believe that each person has a unique tolerance to foods. If you believe that you are not tolerating dairy (or any other food!), our team of Dietitians are here to help you navigate your dietary choices in a way that makes you feel your best while obtaining the key nutrients you need to thrive!
Bottom-line: Enjoy high-fibre and fermented foods daily to support a healthy gut microbiome and reduce inflammation.
2. EAT A RAINBOW OF VEGETABLES AND FRUITS
Higher intake of fruits and vegetables may be a delicious way to reduce inflammation and support immune health! Fruits and vegetables provide fibre, which as we previously discussed can exert anti-inflammatory properties by supporting the gut microbiome. Furthermore, plants contain antioxidants and phytonutrients that have been researched to reduce inflammation:
- Phytonutrients: Also known as phytochemicals, these compounds are found in plant foods that have anti-inflammatory benefits. Flavonoids are one type of phytochemical particularly well-known for their anti-inflammatory potential.
- Antioxidants: These components of plant foods work to protect our bodies from oxidative damage by stabilizing damaging free-radicals. Examples of antioxidants include vitamins A, C, E, and the mineral selenium.
NOTE: "Antioxidant" is a general term for any compound that can counteract unstable molecules called free radicals that damage DNA, cell membranes, and other parts of cells. Because free radicals lack a full complement of electrons, they steal electrons from other molecules and damage those molecules in the process. Antioxidants neutralize free radicals by giving up some of their own electrons. In making this sacrifice, they act as a natural "off" switch for the free radicals.
Tip: In addition to enjoying fruits and vegetables at most meals, you might aim to include two or more colours to your plate in order to obtain a variety of unique phytochemical and antioxidants found in produce.
Let’s explore the unique profile of each colour of vegetables and fruit in the context of its phytochemical and antioxidant content:
- Red: Lycopene is an antioxidant found in red foods like tomatoes, apples, red bell peppers, and watermelon.
- Green: Indoles are found in green foods like kale, spinach, and broccoli.
- Yellow/Orange: Beta-carotene is an antioxidant found in orange/yellow foods like carrots, sweet potatoes, oranges, and squash.
- Blue/Purple: Anthocyanins can be found in purple/blue foods like blueberries, blackberries, grapes, plums, purple cabbage, and even beans and lentils with a purple hue like black beans and kidney beans.
- White: Organosulfur, quercetin, and gingerol are found in garlic, onions, and ginger respectively.
The aforementioned antioxidants and phytonutrients provide only a brief overview of the numerous compounds found in vegetables and fruits which have been linked to reducing inflammation in the body.
Bottom-line: Enjoy a variety of brightly coloured vegetables and fruits as often as possible!
3. BALANCE YOUR BLOOD SUGARS
Diets with relatively high glycemic index and glycemic load have been associated with an elevated risk of inflammatory chronic conditions and markers of inflammation. Carbohydrates that are rich in fibre have a lower glycemic index, meaning that the breakdown of sugar (i.e., glucose) from the food source is delayed. Furthermore, the addition of protein and/or fat to the meal can lower the glycemic load to prevent pro-inflammatory spikes in blood glucose levels.
At Vitality Nutrition, our Registered Dietitians teach a unique meal-building concept called the Fundamental Four that focuses on building meals around four food groups that – when paired together – balance blood sugars. Let’s explore:
- Fibre-Filled Carbohydrates: Oats, fruits, sweet potatoes, squash, beans and lentils, high-fibre grains like popcorn, Wasa crackers, multigrain bread, popcorn, quinoa, brown rice, and barley.
- Proteins: Lean meats and poultry, fish, beans and lentils, eggs, egg whites, high-protein dairy like Greek yogurt, Skyr yogurt, and cottage cheese, and high quality protein powders.
- Fats: Nuts and seeds, nut butters, cheese, avocado, olives, dark chocolate, coconut milk, and oils and fats like avocado oil, olive oil, and butter.
- Volume: Any non-starchy vegetables or lower-carbohydrate fruits like berries.
When combining these food groups thoughtfully on your plate, you'll be nourishing your body with beneficial fibre, phytochemicals, and antioxidants – all of which play a role in reducing inflammation. Furthermore, this combination of food groups supports a steady rise and fall of blood sugars, which is a key consideration in preventing inflammation.
Bottom-line: Choose fibre-filled carbohydrates as often as possible, whilst including protein and fats, as an effective strategy to reducing detrimental spikes in blood sugar levels.
4. SPICE UP YOUR LIFE
Herbs and spices can infuse tasty flavours and aromas into food and are also packed with antioxidants and phytonutrients known to have anti-inflammatory properties.
More recently though, some have become better known for their potential benefits such as cloves, cinnamon, oregano, rosemary, thyme, and turmeric:
- Cloves: The anti-inflammatory properties in cloves may be in part due to a component called eugenol.
- Cinnamon: There is mild evidence that cinnamon can offer anti-inflammatory benefits and one study found that consumption of cinnamon led to lower circulating glucose levels.
- Oregano: A flavonoid called luteolin in oregano has shown a promising anti-inflammation power.
- Rosemary: Contains a variety of phytochemicals with potential roles in anti-inflammation and pain relief.
- Thyme: Made up of anti-inflammatory and antioxidant components, such as thymol, thyme is thought to have the potential to positively impact bacterial growth.
- Turmeric: A component of turmeric, called curcumin, has shown anti-inflammatory effects, such as relieving arthritis or joint inflammation.
Bottom-line: Flavour your meals with spices and herbs as a way to increase the antioxidant and phytonutrient content of your diet.
5. INCLUDE OMEGA 3 FATS
Foods high in omega-3 fatty acids have been associated with anti-inflammatory benefits. When discussing omega 3 fats, we consider the difference between marine and plant sources of omega 3s.
- Marine life: There are two kinds of omega-3 fatty acids found in marine life like fish, algae, and supplements – eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA).
- Plant sources: The form of omega-3 in plant foods like walnuts, chia seeds, hemp hearts, and ground flax is called alpha-linolenic (ALA).
While we encourage the consumption of plant foods that contain ALA, it is important to note that the conversion to anti-inflammatory EPA and DHA is inefficient in humans. Therefore, plant-forms of ALA are not a reliable source of the biologically important EPA and DHA omega 3s in the context of reducing inflammation.
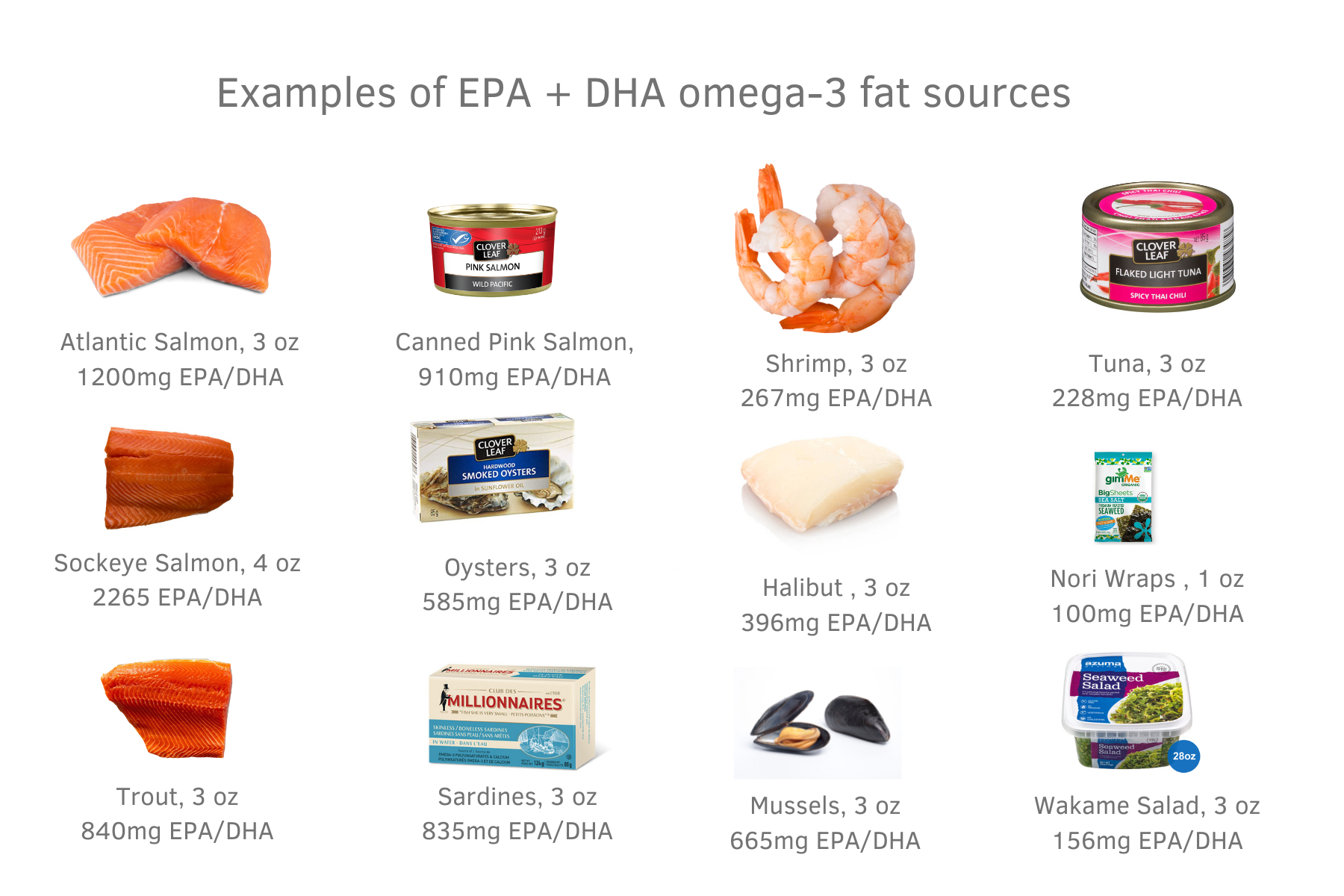
Looking for ways to add omega-3s to your diet? Try our recipes for Poke Bowls, Simple Lemon Butter Salmon, Sockeye Salmon Burgers, or Air-Fryer Halibut with Pineapple Salsa!

What about mercury content of fish? Most of the omega-3 rich fish sources are low in mercury. Furthermore, most of the fish we consume in Saskatchewan is low mercury! Albacore tuna (white tuna) and bluefin tuna are higher in mercury but more commonly consumed forms of tuna like skipjack tuna and light tuna are lower in mercury. High mercury fish that should be consumed less often and avoided in pregnancy are fish that are further up the food chain and include:
- Shark
- Ray
- Swordfish
- Barramundi
- Orange roughy
- Ling
- Bluefin tuna
- Albacore (white) tuna
Bottom-line: Aim to enjoy fatty fish like salmon, trout, and sardines as often as possible and/or consider an omega-3 supplement sourced from fish or algae.
6. LIMIT OMEGA-6S
In contrast to omega-3 fats, omega-6 fats (i.e., arachidonic acid) have been associated with increased inflammation. Omega-6 is found in oils such as sunflower oil, soybean oil, safflower oil, corn oil, and grapeseed oil. Restaurant meals, deep fried foods, commercial baking, and processed foods tend to be high in omega-6s because omega-6-rich oils are used in their production.
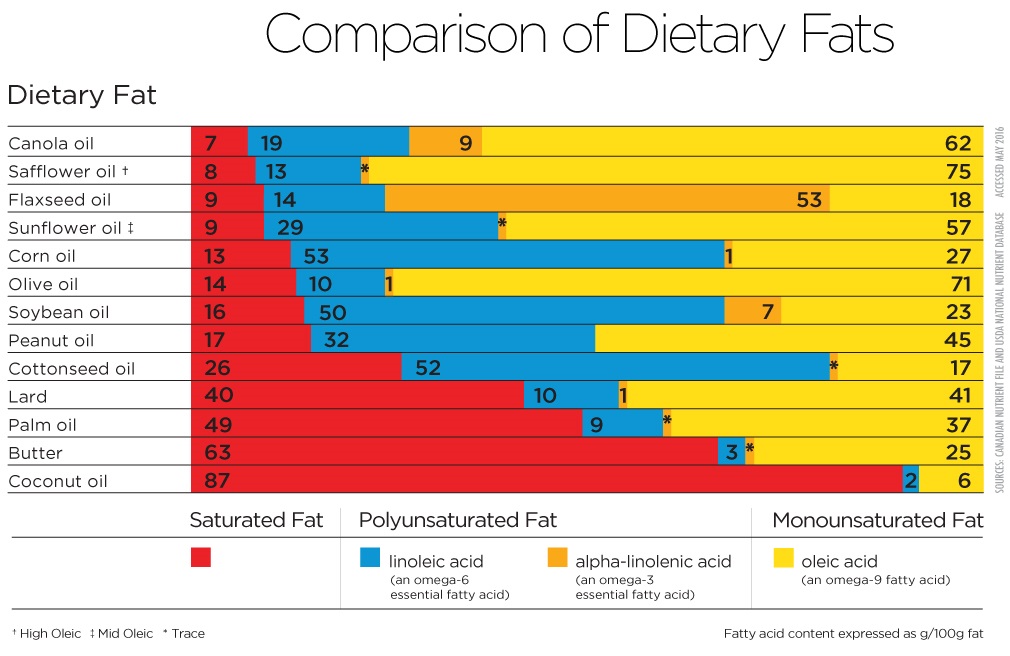
Photo credit to Canola Growers. NOTE: each oil has a blend of fatty acids. While we need some omega 6 fatty acids, choosing oils will less omega 6 (shown in blue) is favorable.
It is also important to note that omega 3s compete for the same pathway as omega 6s. Therefore, reducing the ratio of omega 6s to omega 3s is favourable in the context of lowering inflammatory biomarkers.
Tip: Reduce your omega-6 consumption by cooking with a variety of oils and fats that are low in omega 6 like avocado oil, olive oil, butter, or coconut oil. You might even consider making homemade versions of your favourite baked foods or fried foods so that you can choose oils that do not promote inflammation.
Bottom-line: Limit omega-6s oils in the diet when possible to achieve a more favourable ratio of inflammatory omega 6 oils compared to anti-inflammatory omega 3 fats.
BONUS TIP: AIM FOR WHOLE FOODS FIRST
As our Registered Dietitians will share with their clients, highly processed convenience foods are typically higher in inflammatory omega 6s fats and lower in fibre and protein, making them more likely to spike blood sugars and promote inflammation. Furthermore, they may be processed in a way that reduces their natural nutrient density and displaces the consumption of less-processed options that would offer antioxidants, vitamins, minerals, and fibre.
That being said, one of our core philosophies at Vitality Nutrition is to focus on adding nutritious foods to the diet rather than fixating on the foods we ought to be eating less of. We find that this “add” mindset is a more motivating way to make meaningful changes to our diet that offer anti-inflammatory benefits!
Dietitian Note: Many foods that have a pro-inflammatory nutrition profile can also offer a connection point for friendship, family, experiences, and memories. For this reason, our Registered Dietitians encourage that their clients reflect on our core nutrition philosophy “fuel the body, feed the soul” to determine when less nutritious foods may enhance their quality of life.
Bottom-line: Focus on building your diet around whole foods sources of grains, starches, proteins, vegetables, and fruits to reduce inflammation and naturally displace pro-inflammatory, processed foods.
ADDITIONAL LIFESTYLE CONSIDERATIONS
ENJOY MOVEMENT
Research has shown that an inactive lifestyle may increase the risk of inflammatory-related diseases. Other studies have found that just 20 minutes of exercise a day can be enough to produce an anti-inflammatory response.
Some ways to enjoy exercise might be:
- Going for walks, runs, hikes, or bike rides
- Signing up for a workout class
- Playing sports
- Adopting a strength training regime
Additional considerations should include the type, intensity, and duration of the exercise chosen. As one study found, long periods of intense exercise can lead, in general, to higher levels of inflammatory mediators, and thus might increase the risk of injury and chronic inflammation. By contrast, moderate exercise or vigorous exercise with appropriate resting periods can achieve maximum anti-inflammatory benefits.
DON'T FORGET TO TAKE REST DAYS!
Working-out increases beneficial, acute inflammation in the body which serves to build and repair muscle tissues. While exercising is key for stressing the body in a way that provides positive adaptation, it is equally important to schedule rest days that offer your body the time it needs to heal and repair.
EAT UNTIL SATISFIED
Overnutrition is responsible for elevated levels of glucose and free fatty acids in blood which increase the expression of pro-inflammatory biomarkers. While occasionally over-eating will not lead to chronic inflammation, longer periods of overnutrition can contribute to insulin resistance which increases oxidative stress and promotes inflammation. At Vitality Nutrition, we help our clients understand their unique body signals that tell them when they are hungry and when they are satisfied. Tuning into your body signals is one way to regulate your caloric intake! Some tips to consider if you find yourself eating past satisfied:
- Slow down your eating speed to tune into the signs and signals that tell you that you are transitioning from hungry to satisfied or politely full.
- Take a break at the halfway point of your meal to assess your hunger and fullness cues.
- Eat electronic-free or with others whenever possible which tends to slow down eating speed and limit distractions that can disconnect you from tuning into your body's cues.
LIMIT ALCOHOL
Although it's true that red wine may play a role in decreasing inflammation, it's generally recommended to limit excessive alcohol intake. Excess alcohol has been found to impair liver function, which is a part of our body responsible for getting rid of toxins. Alcohol can also disrupt other general bodily functions and in turn promote inflammation.
MANAGE STRESS
Excessive stress can contribute to inflammation and can even alter food preferences in ways that increase the consumption of more pro-inflammatory choices. We're all unique when it comes to which stress management techniques work best, and working with a healthcare professional for ongoing support is advised when needed.
PRIORITIZE SLEEP
Good quality and quantity of sleep can help us feel fuelled and energized. A disturbed sleep pattern or overly long rest has been associated with signs of increased inflammation. As part of our Comprehensive Nutrition Coach program, we work closely with our clients to adopt nutrition and lifestyle habits that promote restorative sleep!
AVOID INDIVIDUAL FOOD INTOLERANCES & ALLERGIES
As our team of Registered Dietitians know, there is no ‘one-size fits all’ approach to nutrition. For example, consuming garlic may reduce inflammation for some due to its phytonutrient content, but promote inflammation in people with irritable bowel syndrome who do not tolerate high FODMAP foods. Furthermore, fermented dairy may offer anti-inflammatory properties by supporting the gut microbiome for some, but increase markers of inflammation in others with dairy allergies. Consulting with a Registered Dietitian – like those at Vitality Nutrition in Saskatoon – is recommended when identifying food allergies and intolerances.
CONSULT WITH A DIETITIAN BEFORE ADOPTING AN INTERMITTENT FASTING SCHEDULE
As Registered Dietitians, we are often asked whether intermittent fasting is a recommended strategy for reducing inflammation.
Time-restricted eating is a form of intermittent fasting that involves confining one's eating window and fasting for the remaining hours of the day. Some research has found that eating within this shortened window can reduce markers of oxidative stress. One study found that consuming all calories within an 8-hour window each day, in conjunction with resistance training, improved some biomarkers of inflammation.
That being said, in some cases, restricting your eating to a condensed window can be difficult to fit into your lifestyle, can cause you to miss out on opportunities to consume beneficial nutrients, may negatively impact hormone function, and may not provide the energy you require for your workouts and lifestyle. In other cases, we’ve found that adopting strict nutrition protocols like intermittent fasting can negatively impact your mindset and leaded to disordered eating patterns. For these reasons, we recommended consulting with a Registered Dietitian before adopting an intermittent fasting or time restricted eating regime to ensure that this approach is in alignment with your nutrition and lifestyle goals.
CONCLUSION
Adopting nutrition and lifestyle habits that have anti-inflammatory properties is one way to protect the body from the harmful long-term effects of inflammation. The team of Registered Dietitians at Vitality Nutrition in Saskatoon are here to help provide individualized and evidence-based recommendations to reduce inflammation using the power of nutrition and lifestyle. You can take action and combat chronic inflammation with the following seven habits:
- Support your gut by eating fibre and fermented foods
- Eat a rainbow of veg and fruit
- Balance your blood sugar with the four food groups
- Add spices and herbs when cooking
- Include omega-3 rich marine life like fatty fish
- Limit omega 6 oils when possible
- Build the base of your diet around whole foods.
Ready to bring the evidence-based nutrition support of our Registered Dietitians into your kitchen?
Hungry for more?
Get recipes, tips, and updates from the Vitality Nutrition team straight to your inbox!
Don't worry, your information won't be shared.

