A Dietitian's Guide to Nutrition in Pregnancy
Oct 19, 2022
Our team of Registered Dietitians in Saskatchewan have curated this guide to nutrition during pregnancy for anyone who is pregnant, is looking to become pregnant, or is supporting someone through a pregnancy!
Having a baby can be a wonderful experience but also can be a time of uncertainty. Many parents have questions and concerns regarding food and supplement intake. With advice coming from many sources, it is tough to know who to listen to. That is why having accurate nutrition information from Registered Dietitians is so important! This article is prepared with information as you navigate nutrition needs before and during pregnancy.
In this guide, we’ll uncover three key nutrition discussions:
- Key nutrients to consider during pregnancy and how to source them through food.
- Which foods, beverages, and supplements to avoid to ensure a safe pregnancy.
- How to use nutrition to overcome symptoms such as morning sickness, heartburn, constipation, and more.
You can listen to the podcast episode that accompanies this article here.
1. KEY NUTRIENTS TO CONSIDER
All of the vitamins and minerals needed for healthy adults are important to obtain during pregnancy. However, a few key nutrients including energy, protein, folate, iron, omega-3s, and choline are needed in additional quantities. Let's explore the important of these pregnancy supportive nutrients and how to source them through food and pregnancy approved supplementation.
TOTAL ENERGY (CALORIES)
Consuming enough energy (ie. calories) is one of the most crucial nutrition considerations during pregnancy to ensure that mom and baby have the resources needed for optimal growth and development.
Many authorities offer calorie recommendations for mother’s to follow. For example:
- 1st trimester: calorie needs the same as pre-pregnancy
- 2nd trimester: calorie needs increase by about 340 calories
- 3rd trimester: calorie needs increase by about 450 calories

While these calorie recommendations may be helpful for some, we do not find the application to be helpful for all mom’s. Instead, we guide mom’s towards additions to meals or snacks to boost their nutrition so that they can develop an eating pattern that supports them through pregnancy. Some tips to obtain adequate energy:
- EAT REGULARLY: having a meal or snack every 2-3 hours can ensure you meet your energy needs across the day while also helping to manage common symptoms discussed below (ie. heartburn and nausea).
- ADD SNACKS: adding snacks is an important way to boost your energy intake without feeling too full which can trigger symptoms like nausea or heartburn.
- BALNCE YOUR MEALS: energy (ie. calories) can be obtained from carbohydrates, fats, and proteins. Building fats, carbs, and proteins into all of your meals and snacks is an important way to obtain the energy you and baby need to thrive!
- LISTEN TO YOUR CUES: Tune into your body and listen to your hunger and fullness cues to decide when and how much to eat. Keep in mind that food aversions or other symptoms can deter you from eating. Especially in the first trimester. In this case, mechanical eating (ie. eating every 2-3 hours even in the absence of hunger cues) could be an essential strategy to ensure you obtain the nutrition you and baby need!
Your doctor will monitor your weight gain to ensure that you are eating enough and gaining the healthy weight that you and baby need to thrive. There are clinical guidelines for weight gain through pregnancy that are associated with the best health outcomes. You can review these recommendations in the graphic below:
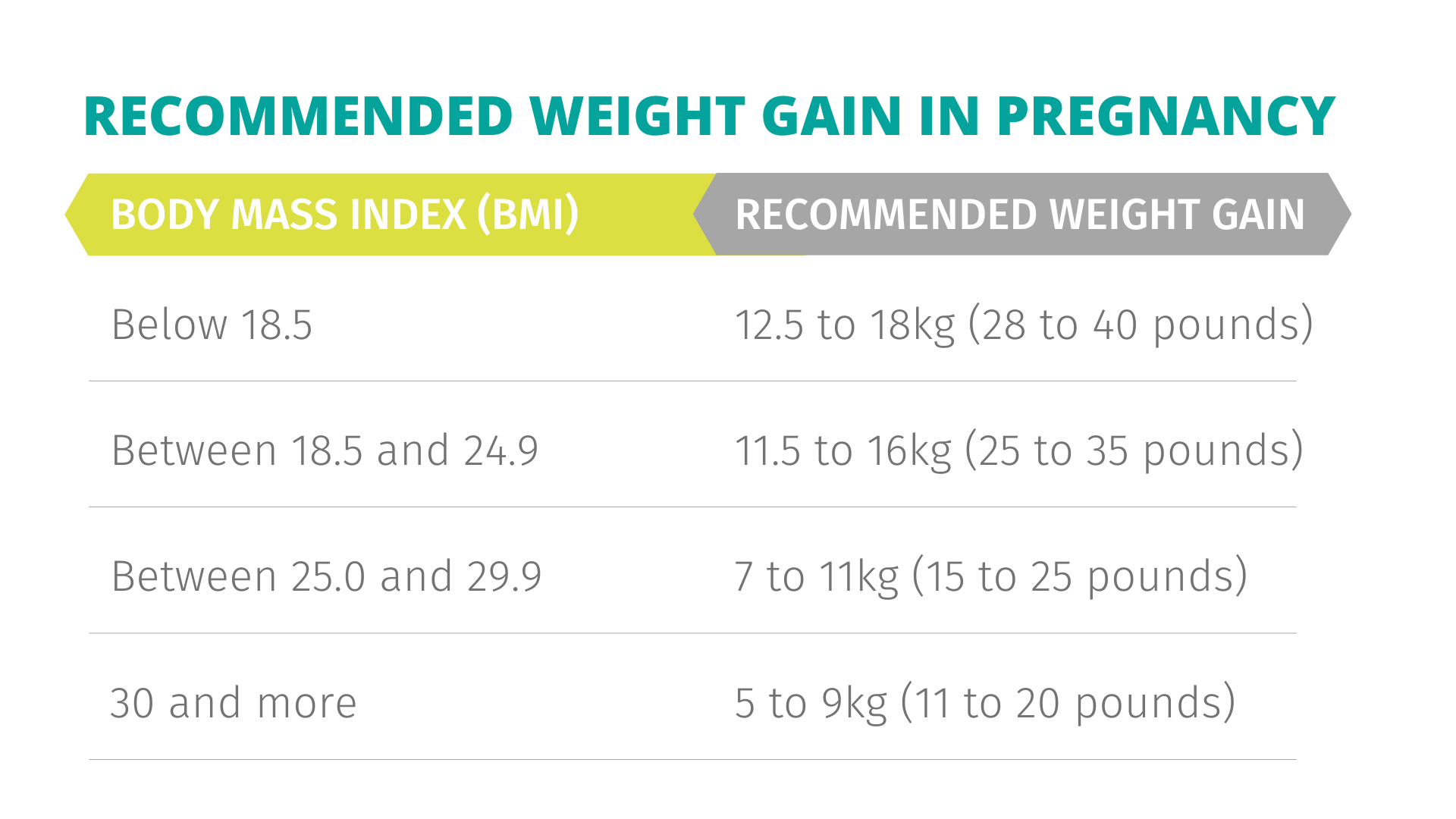
DIETITIAN NOTE: Weight gain can be an emotionally charged experience as the body rapidly adapts to the needs of the growing fetus. If monitoring weight changes would compromise your ability to make nourishing food choices then we recommend having a discussion with your doctor. You can ask your doctor not to share your specific weight and instead let you know if you are on track towards healthy weight gain. From there, your doctor can direct you towards any adjustments that may be necessary to keep you and baby well and nourished.
PROTEIN
Protein requirements increase throughout pregnancy due to an exponential increase in growth for both mom and baby’s tissues. The recommended daily protein intake is a minimum of 1.1g/kg of protein. For example, for a 150 pound or 68kg person this would be at least 75g of protein daily.

Rather than tracking specific protein intake, we recommend that women build protein foods into meals and snacks to ensure they get enough! The habit of building protein-containing foods into meals and snacks ensures adequate protein intake, helps to keep blood sugars stable to manage common pregnancy symptoms like nausea, and offers key vitamins and minerals like iron.
COMMON QUESTION: is protein powder safe during pregnancy?
Many people enjoy using protein powders and bars as a protein source in their day. While protein powders and bars aren’t necessary to meet your protein needs in pregnancy, they may be protein sources that you enjoy using. There are no dangers to protein powders including whey isolate, casein, whey concentrate, or plant-based options. However, the supplement industry is not regulated by Health Canada so it isn’t often clear (or reliable) that what is in the supplement is safe during pregnancy. Unlike whole food sources of protein, protein powders can contain trace amounts (or have cross contamination) of heavy metals, stimulants, or herbs that are unsafe for expecting moms. For this reason, we recommend checking with your dietitian or physician regarding any protein powders, shakes, or bars you plan on using to ensure they are safe for you to consume!
DIETITIAN'S KEY TAKEAWAY: Build protein foods into meals and snacks to obtain the protein and key micronutrients that you and baby need through pregnancy.
FOLATE (FOLIC ACID)
Folate, also known as folic acid, assists in the development of the brain and spinal cord. Folate is especially important to prevent neural tube defects in the developing fetus. The neural tube forms in the embryo between the 17th to 30th day after conception. In many cases, this important milestone occurs before mom even knows she is pregnant!
Folate is the ‘natural’ form of the vitamin which is found in dark green vegetables, citrus fruits, peanuts, beans and lentils, whole grain, seafood, and liver. Folic acid is the synthetic form which is found in supplements and fortified food like white flour and cereals. Health Canada requires mandatory fortification of white flour as a preventive measure for neural tube defects. It is recommended that women wanting to get pregnant supplement with at least 400mcg of folic acid each day to help prevent birth defects. Review the label of your prenatal multivitamin to ensure it has at least 400mcg of folic acid!
HOW MUCH YOU NEED: 400mcg before pregnancy and 600mcg during pregnancy
SOURCE: green leafy vegetables, citrus fruits, peanuts, beans and lentils, whole grains, seafood, liver, and fortified foods like white flour or any food made with white flour and cereals, and a prenatal supplement.
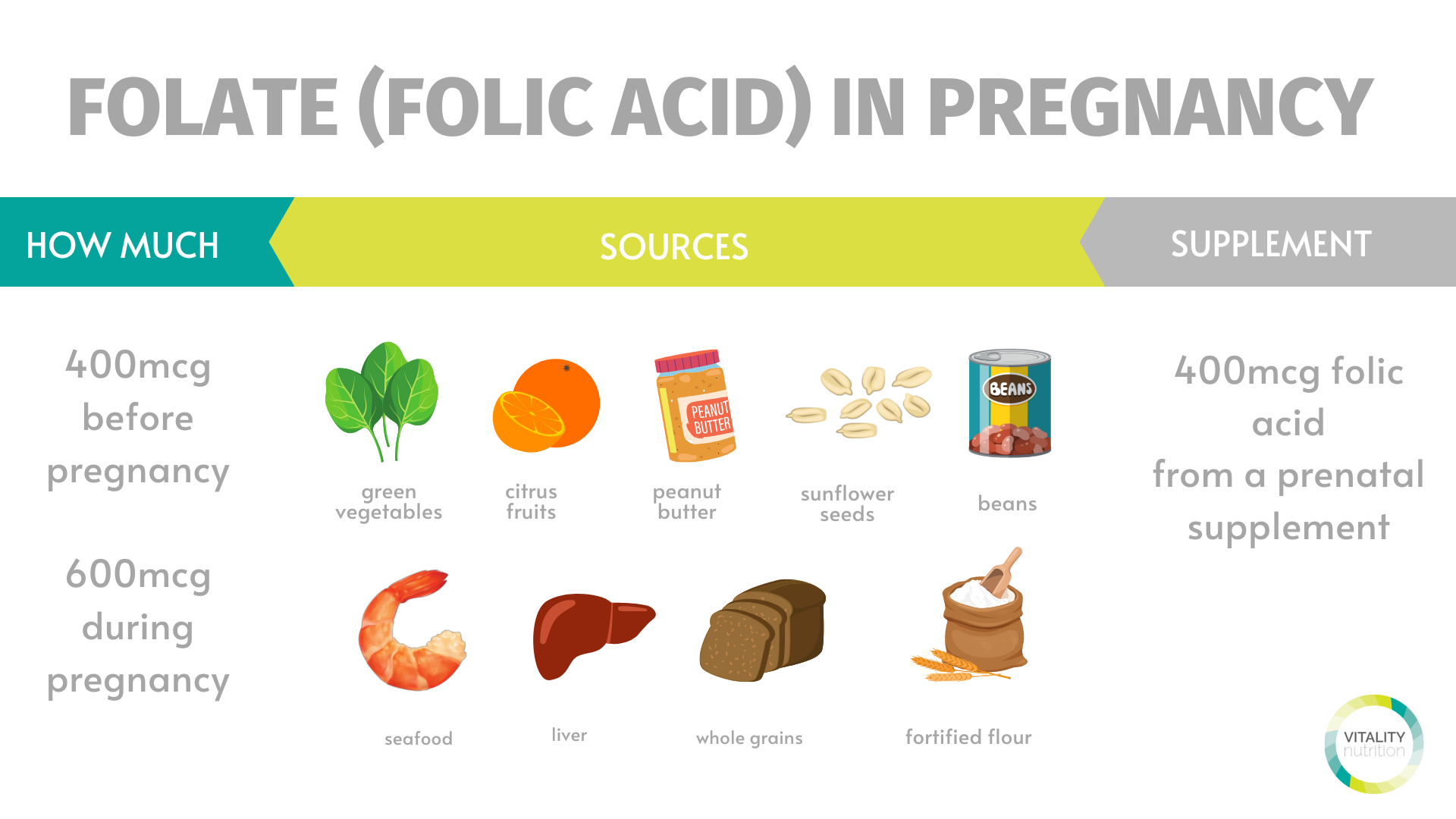
DIETITIAN'S KEY TAKEAWAY: supplement with at least 400mcg of folic acid if you are wanting to get pregnant or are pregnant and prioritize folate rich food sources.
IRON
The body uses iron to make hemoglobin. Hemoglobin is a protein in the red blood cells that carries oxygen to the body's tissues. During pregnancy, you need double the amount of iron that nonpregnant women need. Your body needs this iron to make more blood to supply oxygen to your baby!
If you don't have enough iron stores or get enough iron during pregnancy, you could develop iron deficiency anemia. Severe iron deficiency anemia during pregnancy also increases the risk of premature birth, having a low birth weight baby, and postpartum depression. Furthermore, mom’s iron stores are passed onto the baby which baby requires for the first 4-6 months of life before starting iron-rich solid foods.
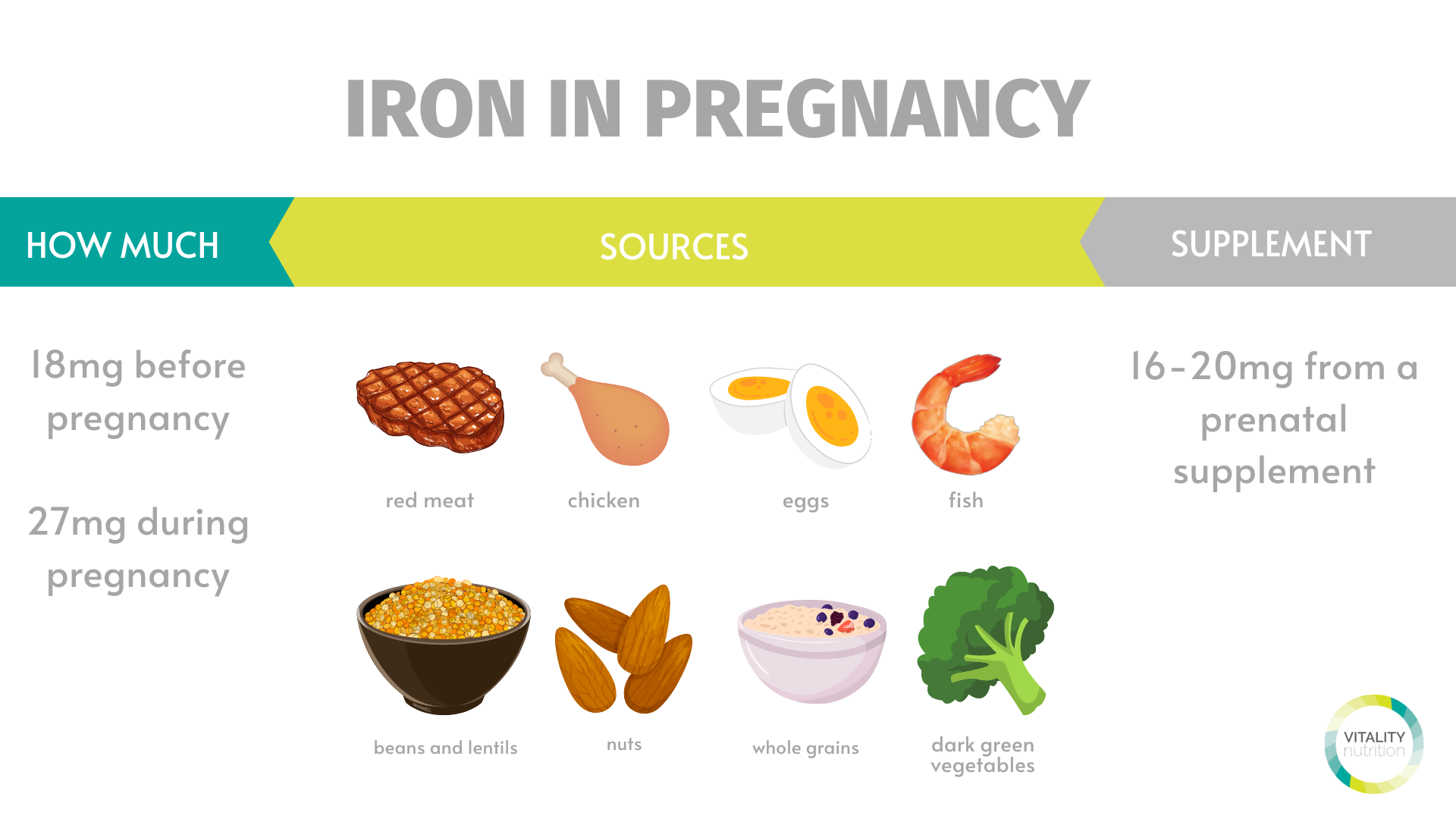
It is recommended that women consume iron-rich food sources and also supplement with a prenatal supplement that contains 16-20mg of iron. Iron-rich food sources from animals such as meat, poultry, and eggs are the most readily absorbed. Plant-based sources like beans and lentils, leafy green vegetables, and some whole grains aren’t as easily absorbed. To enhance the absorption of iron from plant sources and supplements, pair them with a food high in vitamin C such as citrus fruits, strawberries, tomatoes, bell peppers, kiwis, or broccoli.You can learn more about iron via this blog and listen to our podcast episode on iron here.
HOW MUCH YOU NEED: 27 milligrams a day
SOURCES OF IRON: beef, poultry, game meat, lamb, eggs, and plant-based sources like beans and lentils, nuts and seeds, green leafy vegetables, and some whole grains.
DIETITIAN'S KEY TAKEAWAY: iron is an important mineral during pregnancy and it is recommended that expecting moms supplement with a prenatal that contains between 16-20mg of iron and also source iron-rich foods in their diet.
OMEGA 3s
Omega-3 fatty acids that play a critical role in optimal health and requirements are thought to increase during pregnancy. The most biologically active forms of omega-3s are docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA), which are primarily derived from marine sources such as seafood and algae. During pregnancy, DHA is transferred from the mother across the placenta and accumulates in the growing fetal brain and other tissues. After birth, DHA is transferred through breast milk. DHA helps to support:
- brain development
- eye development
- nervous system development
The omega-3s may also prevent preterm labor, ensure a healthy birth weight, and support a mother’s mood during the postpartum period.
The richest sources of these omega-3 fatty acids are marine sources, such as seafood and omega-3 fish oil or algae supplements. To optimize pregnancy outcomes and fetal health, consensus guidelines have recommended that pregnant women consume two servings of fish per week to obtain their omega-3 requirements. Some women may consider supplementing with at least 200mg of the fatty acid DHA if they do not regularly consume seafood.

COMMON QUESTION: what about plant based sources? Algae is a plant-based source that contains the biologically active forms of the omega-3 fatty acids discussed (ie. EPA and DHA). Other sources of omega-3 fatty acids such as flax seed oil, walnuts, and vegetable oils, however, contain ALA that needs to be converted to longer-chain EPA and DHA to become biologically useful. This conversion is inefficient in the body meaning that these sources are not reliable to ensure adequate EPA and DHA is consumed through the diet.
DIETITIAN KEY TAKEAWAY: pregnant women require omega-3 fatty acids which can be obtained by ingesting two servings of omega-3 rich fish per week and/or supplementing with an omega-3 fish oil supplement or prenatal supplement with at least 200mg of DHA.
COMMON QUESTION: what about the mercury content of fish?
Mercury found in some fish sources can be toxic to humans and the developing fetus. It is advised that all people consume no more than two servings of high mercury containing fish per week and to completely avoid high mercury containing fish when pregnant. Predatory fish typically contain the most mercury as it accumulates in their body with size and age. These fish include shark, orange roughy, swordfish, and ahi or albacore tuna. Light tuna or skipjack tuna are low in mercury.
CHOLINE
The importance of ensuring adequate choline intakes during pregnancy is increasingly recognized as choline plays a critical role in processes including brain development and gene expression. Experts recommend that pregnant women get slightly more choline than non-pregnant women at 450 mg of choline each day. Although the body produces some choline on its own, it doesn’t make enough to meet all your needs while you are pregnant. Many prenatal supplements do not contain chlorine and it is important that women source enough through food sources. Choline can be found in eggs, liver, beef, cod, soy products, potatoes, beans, and milk.
Our team of Registered Dietitians in Saskatchewan touched on nutrients that are needed in increased quantities during pregnancy including energy, protein, folate, iron, omega-3, and choline. However, all vitamins and minerals are required to keep you thriving during your pregnancy. Additional nutroents including vitamin D, calcium, B vitamins, and electrolytes can be obtained by eating a whole food, nutrient-dense diet and taking a prenatal supplement.
2. WHAT TO LIMIT OR AVOID
The Registered Dietitians at Vitality Nutrition believe in a concept called the 'add mindset' when it comes to making supportive nutrition changes. While this mindset has application during pregnancy as discussed above, there are certain food, beverages, and supplements that need to be limited or avoided to keep mom and baby safe and well. Let's explore recommendations around caffeine, alcohol, foods at a high risk of foodborne illness, herbal teas, and supplements.
CAFFEINE
A reduction or elimination of caffeine during pregnancy is important because:
- Caffeine’s metabolic rate in mothers is significantly decreased, especially after the first trimester
- Caffeine crosses the placenta to your baby and the fetus does not have the enzymes needed to metabolize caffeine.
- Caffeine consumption during pregnancy is associated with low birth weight, decreased fertility, fetal growth restriction, increased risk of miscarriage, and increased risks to baby including cognitive development impairments.
The research regarding safe levels of caffeine consumption for women is conflicting. Health Canada recommends that pregnant women consume no more than 300mg of caffeine per day. Other authorities recommend no more than 200mg per day based on potential complications mentioned above. Other research highlights that there may not be a safe level of caffeine consumption during pregnancy due to consumption of 100mg being correlated to complications. Therefore, mothers who consume more than 300mg of caffeine are encouraged to reduce or completely eliminate their caffeine consumption. However, even this dosage is being reevaluated based on increasing evidence, which has shown that even daily doses of less than 100 mg may cause complications.

It’s important to note that caffeine is found in more than just coffee but can also be ingested from tea, soda, chocolate, energy drinks, or pre-workout supplements. Furthermore, the amount of caffeine in your coffee or tea can depend on the serving size, the brand, or how it was brewed. Account for all of your caffeine sources when keeping track of your total consumption!
DIETITIAN'S KEY TAKAWAY: reduce caffeine consumption to no more than 300mg per day.
ALCOHOL
The safest choice for a woman who is pregnant or planning to become pregnant is not to drink alcohol. Alcohol consumption can be harmful at any point throughout your pregnancy because your baby's brain and central nervous system are under development during this time. If you are finding it difficult not to drink alcohol in pregnancy, reach out to a healthcare professional who can help you get the support you need.
FOODS AT HIGH RISK OF FOODBORNE ILLNESS
Health Canada recommends avoiding foods that have a high risk of foodborne illness as getting food poisoning is problematic to the health of the baby. Because of all the changes happening in your body, you and your unborn baby are at an increased risk of food poisoning. Your immune system is weakened, so it could be harder for you to fight off infections. Some bacteria, such as Listeria can go through the placenta. So if you become sick, there is an increased risk that your baby could get infected. Baby’s immune system is not developed enough to fight off harmful bacteria.

You can lower your chance of getting food poisoning by avoiding the following foods or preparing them in a food safe way.
|
Raw fish, meat, or poultry (eg. such as sashimi, raw oysters, pâté, smoked fish, etc.). |
Fully cooked fish and meat (eg. shrimp sushi rolls) |
|
Soft cheeses (eg. brie, camembert, havarti, and stilton) |
Choose hard cheese instead |
|
Raw or unpasteurized dairy products like milk or cheese |
Choose pasteurized versions |
|
Unpasteurized juices (eg. unpasteurized apple cider) |
If you are consuming unpasteurized juice, bring it to a boil and let it cool before consuming. |
|
Raw sprouts (eg. bean sprouts, alfalfa, mung beans) |
Cook sprouts if you wish to have them! |
|
deli-meats (eg. bologna, roast beef, ham turkey breast, and hot dogs) |
If you want to enjoy deli meats or hot dogs, fully heat them before eating. |
|
raw or lightly cooked unpasteurized eggs or foods that contain unpasteurized raw eggs (eg. homemade Caesar vinaigrette, cookie dough, cake batter, sauces). |
Purchase pasteurized eggs which decreases the risk for foodborne illness. However, it is still recommended to fully cook eggs during pregnancy and avoid foods with raw eggs (eg. salad dressing, cookie dough, or eggnog). |
Health Canada has a complete guide to safe food handling which you can find here.
HERBAL TEAS
Drinking certain herbal teas, including chamomile tea, may not be safe for your baby. Chamomile has been used to stimulate uterine contractions in pregnant women which could potentially lead to a higher incidence of preterm labor. For now, we do not know if chamomile can cause contractions at a point in pregnancy and studies on this would be difficult to conduct for ethical reasons. Until further research can prove that chamomile is safe to take while pregnant, it is safest to abstain from it.
TEAS TO AVOID: chamomile, aloe, coltsfoot, juniper berry, pennyroyal, buckthorn bark, comfrey, labrador tea, sassafras, duck root, lobelia, stinging nettle and senna leaves.
TEAS THAT ARE SAFE: citrus peel, ginger, orange peel and rose hip
SUPPLEMENTS
It is recommended that women looking to conceive and pregnant women take a prenatal vitamin with at least 400mg of folic acid and 16-20mg of iron. A prenatal with vitamin D or separate vitamin D supplement is recommended for women to meet their vitamin D needs. This is not related to an increased need for vitamin D but difficulty for all Canadians in obtaining adequate vitamin D through foods and inadequate exposure to the sun during the winter months.
Aside from a prenatal supplement and vitamin D, it is recommended that women do not take additional supplements. This is because most dietary supplements are not reviewed by Health Canada for their safety and efficacy. Furthermore, it is unethical to test supplements on pregnant women which is why most supplements (eg. protein powder) will state “not safe for pregnant women '' on the label.
DIETITIAN KEY TAKEAWAY: take a prenatal supplement with at least 400mcg folic acid and 16-20mg iron. You might also choose to supplement with vitamin D and an omega-3 with at least 200mg DHA. Avoid all other supplements unless approved by your doctor or dietitian.
3. SPECIAL CONSIDERATIONS
Many women experience challenging symptoms in pregnancy including nausea and vomiting, heartburn, constipation, fatigue, and food aversions. Unique nutrition strategies can be adopted throughout pregnancy to manage or eliminate these symptoms!
NAUSEA (MORNING SICKNESS)
Morning sickness is a common symptom of pregnancy and is marked by nausea and occasional vomiting. Despite the name, morning sickness can cause discomfort at any time of the day. Research suggests that nausea and vomiting during pregnancy might be due to the effects of a hormone produced by the placenta called human chorionic gonadotropin (HCG). Pregnant women begin producing HCG shortly after a fertilized egg attaches to the uterine lining. HCG peaks at 12 weeks and then slowly starts to decline. This is why most women who experience an improvement in symptoms after the first trimester. Some nutrition strategies to relieve or reduce nausea:
- EAT IMMEDIATELY UPON WAKING: Blood sugars are more vulnerable during pregnancy due to an increased need for glucose for the developing fetus and changes to your hormone levels. A low blood sugar can cause or exacerbate nausea. Many women find it supportive to eat a small carb snack immediately upon waking to manage nausea (eg. crackers, dried fruit, or toast) and then build in a more balanced mix of food groups 1-2 hours after waking.
- SUPPORT BLOOD SUGARS: While eating a serving of carbohydrates can restore blood sugars and treat nausea, aim to mix food groups together for most meals and snacks to keep blood sugars stable.
- EAT REGULARLY: An empty stomach can make nausea worse. Many women find it supportive to adopt a small, frequent meal structure to avoid an empty stomach. Small meals tend to be supportive to avoid a full stomach which can also make nausea worse.
- SEPARATE LIQUIDS & SOLIDS: Consider drinking water between meals instead of with a meal to avoid feeling too full as being too full can trigger nausea or vomiting.
- TRY ROOM TEMPERATURE OR COLD FOODS: Many women find that cold foods help in symptom management.
- AVOID OFFENSIVE ODOURS: Women have an increased sense of smell through pregnancy so odours that you do not like can be exacerbated and initiate feelings of nauseousness.
- STAY HYDRATED: if dehydration is a concern due to vomiting or an inability to drink and eat then supplementing with electrolytes may be important.
HEARTBURN
Many women experience acid reflux or heartburn in pregnancy. Heartburn is a sensation of burning in the upper part of the digestive tract including the throat. It is caused by an increase in the pregnancy hormone called progesterone which causes the relaxation of the esophageal sphincter. This causes food in the stomach to push against the sphincter and stomach acid to come back into the throat. Not only is this an uncomfortable sensation but it can also discourage women from eating and obtaining the nutrients they need. Some strategies to manage or improve symptoms:
- AVOID FOODS THAT MAKE HEARTBURN WORSE. This can be unique person to person! For example, some women find tomatoes worsen symptoms whereas another might find that it's chocolate.
- EAT SMALL, FREQUENT MEALS: Small meals ensure that your stomach isn’t so full that pressure is placed on the sphincter. Eating frequently is key to obtaining the nutrition you need!
- EAT SLOWLY AND CHEW FOOD WELL: Chewing your food well can help the food you eat move from the stomach to the small intestine to avoid a back-log of food that can place pressure on the sphincter
- DRINK FLUIDS BETWEEN MEALS. Avoiding a full stomach helps to prevent pressure on the sphincter which can aggravate heartburn symptoms.
- AVOID CARBONATED BEVERAGES: Carbonates beverages can contribute to feelings of fullness which triggers acid reflux.
- AVOID LAYING DOWN AFTER EATING: This gives gravity a chance to assist in digestion as food will more easily move from the stomach to the small intestines. If you do need to lay down after eating, try propping your head and shoulders up with a pillow to encourage the downward movement of the contents of the stomach.
- MANAGE FAT INTAKE: Fat slows digestion which can cause food to sit in the stomach for longer and put pressure on the sphincter. Many women find it supportive to avoid high fat or greasy meals when it comes to managing heartburn. Fat is still an important nutrient to consume enough of so we encourage expecting mothers to continue to eat fats but in portions that are supportive in the management of heartburn.
CONSTIPATION
Many women experience constipation in their pregnancy as a side effect of iron supplementation or as part of the digestive changes associated with pregnancy. Constipation is often caused by increased levels of progesterone and a decrease in gut transit time in the second and third trimester. Some strategies to reduce symptoms:
- INCREASE FLUID INTAKE. Drink at least 2.5L of fluids to lubricate the digestive tract and assist in a bowel movement. You may need more than 2.5 L of water if you are more active or have a very high fiber intake. While we recommend choosing water as your main source of fluid, you can also include soups, broths, milk, plant-based beverages, sparkling water, and smoothies.
- EMBRACE MOVEMENT. Embrace movement that is safe during pregnancy to stimulate the bowels to move. Some ideas including walking and swimming!
- INCREASE FIBRE INTAKE. Fiber can help increase gut transit time to relieve constipation. You can read the blog for a complete list of high fiber foods including chia seeds, fruits, beans and lentils, whole grains, and avocado.
COMMON QUESTION: should I add a fiber supplement?
While adding a fibre supplement (eg. Metamucil) is safe during pregnancy, as Registered Dietitians we prefer to support expecting mothers in reaching their fibre intake through natural food sources. If you struggle to obtain enough fibre through diet, consider adding one or more of the very high fibre foods highlighted below. If you still find it difficult to consume enough fibre due to altered food preferences or aversions, then adding a supplement could be an effective tool to support your digestion and meet your fibre requirements!

FATIGUE
Changing hormones and growing a human can decrease energy levels. While additional rest and sleep may be the most effective strategy to manage fatigue, some nutrition and lifestyle strategies to consider include:
- SUPPORT BLOOD SUGARS: Keeping blood sugar level is a supportive strategy for everyone to adopt when it comes to improving energy. However, changes in hormones, symptoms like nausea or heartburn, or food aversions may make it more difficult to build blood sugar supportive meals. Finding sources of fat, protein, and fiber-filled carbs that you enjoy and tolerate is important when it comes to supporting your energy levels!
- EAT ENOUGH. Caloric requirements are increasing through pregnancy. Eating more at meals or adding supportive snacks is a key consideration to support your energy levels.
- STAY HYDRATED: Staying hydrated ensures that nutrients and oxygen can be transported to your brain and muscles. Hydration is one part fluid and another part electrolytes:
- Fluid needs may be increased during pregnancy so continue to focus on hydration to support energy levels. Most women require about 500mL above their baseline or 2 extra cups of water!
- Electrolytes such as sodium and potassium are also important to concern when it comes to staying hydrated. There is a reason women crave salty pickles during pregnancy! In some cases, an increased focus on electrolyte rich foods like condiments for sodium, fruits and veggies for potassium and magnesium, and milk and plant-based alternatives for calcium.
FOOD AVERSIONS
If you were expecting to want to eat everything in sight while pregnant, then your sudden hatred of what used to be your favorite snack might take you by surprise. Food aversions are possibly caused by the hormonal changes of pregnancy. The amount of human chorionic gonadotropin (hCG), the hormone that can also cause nausea, rapidly rises in the first trimester of pregnancy. This is why you’re most likely to experience food aversions during the first trimester. However, you can experience food aversions at any point during pregnancy. Most of the time, food aversions will disappear after your baby arrives. It’s also possible for aversions to continue indefinitely.
The most common food aversions that women have shared with us include meat, eggs, milk, onions and garlic, tea, coffee, and spicy foods. In most cases, it’s healthy to listen to your body during pregnancy. This means that it’s fine to avoid your aversions. If your aversions include foods that are important during pregnancy, make sure you’re getting those nutrients in other ways. For example, if you have an aversion to meat, aim to include other high protein foods like Greek yogurt, cottage cheese, beans and lentils, tofu, higher protein milks, etc. You can also get around aversions by “hiding” the food that you don’t want in other foods. For example, if folate-rich leafy greens turn you off perhaps you could sneak a handful of spinach into your smoothie.
GESTATIONAL DIABETES
During pregnancy, an organ called the placenta gives a growing baby nutrients and oxygen. The placenta also makes hormones that can block insulin to ensure glucose and nutrients are reserved for the fetus. When insulin is blocked, it’s called insulin resistance. If blood glucose goes up to high it can cause gestational diabetes. Screening for gestational diabetes mellitus at 24 – 28 weeks gestation is recommended for all pregnant women, while screening at any stage of pregnancy is recommended for women with a high risk of gestational diabetes mellitus. Individualized nutrition care from a Registered Dietitian for women at risk for or diagnosed with diabetes in pregnancy can promote adequate nutritional intake, achievement of target glucose levels, appropriate maternal weight gain and growth of the fetus.
HYPERTENSION & PREECLAMPSIA
Gestational hypertension is high blood pressure in pregnancy. High blood pressure is a concern as it can be detrimental to the placenta and fetal growth and lead to preeclampsia which can affect blood supply to the placenta and place stress on the mothers organs. Your healthcare team will monitor your blood pressure throughout pregnancy. Gestational hypertension may warrant nutrition intervention. While restricting salt intake is not typically necessary in pregnancy, it may be a consideration if managing blood pressure is a concern.
CONCLUSION
Pregnancy is a critical time in the life cycle for both mom and baby! After a baby is born, nutrition continues to be a high priority with increased energy needs if mom chooses to breastfeed and the unique needs of the infant at 4-6 months when solids are introduced! The Registered Dietitians at Vitality Nutrition are here to support you whether you are looking to understand and support your menstrual cycle to get pregnant, nourish your body during pregnancy, meet the increased nutrition demands when breastfeeding, or to support you as you introduce solids to your infants! To learn more about working 1:1 with a Registered Dietitian in-person in Saskatoon or remotely anywhere across Saskatchewan including Regina, North Battleford, Prince Albert, and more here.
You can find the full podcast episode that accompanies this article here.
Ready to bring the evidence-based nutrition support of our Registered Dietitians into your kitchen?
Hungry for more?
Get recipes, tips, and updates from the Vitality Nutrition team straight to your inbox!
Don't worry, your information won't be shared.

